CMS Finalizes 2026 Home Health Medicare Payment Rule: What the 1.3% Cut Means for Agencies and Your Strategic Response
This comprehensive analysis examines CMS's finalized 2026 Home Health Medicare Payment Rule, breaking down the 1.3% payment reduction and its implications for agency operations. The piece provides strategic guidance for home health leaders navigating ongoing reimbursement pressures while maintaining quality patient care. Readers will discover practical action steps for optimizing operations under the new payment structure and positioning their agencies for long-term success. Essential reading for any home health agency owner preparing for the January 2026 implementation.
12/1/20255 min read
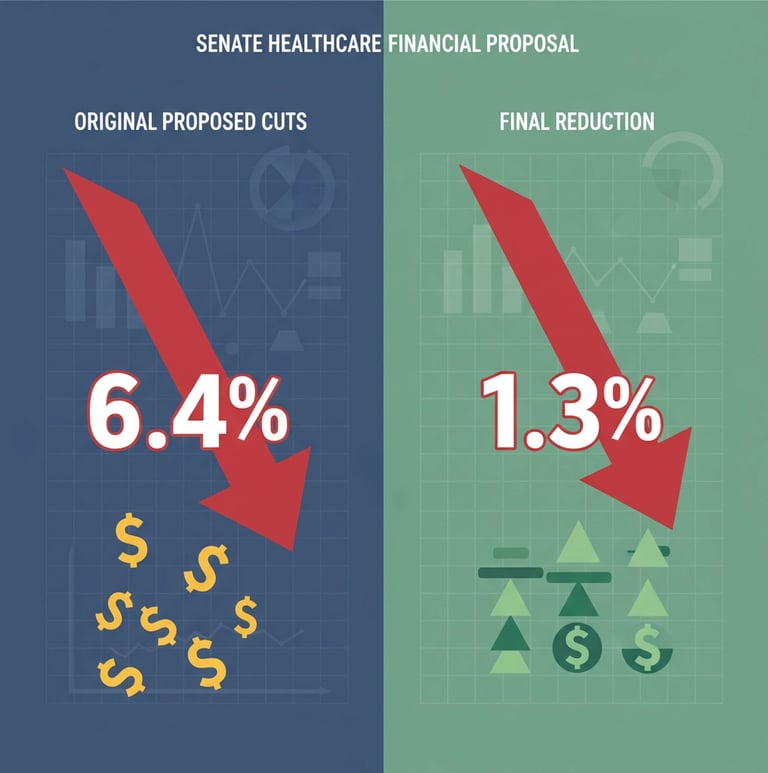
CMS has finalized its 2026 Home Health Medicare Payment Rule with a 1.3% aggregate payment reduction, a significant improvement from the originally proposed 6.4% cut that would have devastated the industry. This final rule represents both a victory for industry advocacy and a continued challenge for home health agencies navigating ongoing reimbursement pressures while maintaining quality patient care.
From Devastating Cuts to Manageable Reductions: What Changed
The transformation from a proposed 6.4% payment cut to a final 1.3% reduction represents one of the most dramatic policy reversals in recent Medicare history. According to the CMS Final Rule fact sheet, this change translates to approximately $915 million more in payments compared to what the original proposal would have delivered.
The final payment structure includes a 2.4% rate increase offset by a 0.9% permanent adjustment and a 2.7% temporary adjustment. In practical terms, agencies will see an average decrease of approximately $19 per 30-day period. While still a reduction, this represents a far more manageable financial impact than the industry initially faced.

The permanent adjustment of -1.023% accounts for differences between assumed and actual behavior changes since the Patient-Driven Groupings Model (PDGM) implementation in 2020. CMS used updated 2024 utilization data to make this calculation more accurate, addressing long-standing industry concerns about outdated assumptions driving payment policy.
Understanding the Broader Reimbursement Landscape
This payment adjustment continues a troubling trend we've discussed in our previous analysis of reimbursement and regulatory updates. The 2026 rule marks the fourth consecutive year of permanent cuts to home health Medicare payments, bringing cumulative reductions to nearly 9% since 2023.
These sustained cuts occur against a backdrop of increasing operational costs, workforce shortages, and rising patient acuity levels. As we explored in our labor shortage crisis analysis, agencies face mounting pressure to maintain service quality while managing tighter margins.
The timing of these cuts becomes particularly concerning when viewed alongside potential broader Medicare reductions. Our recent analysis of Congress's consideration of up to 9% cuts to Medicare and Medicaid shows how agencies must prepare for multiple layers of reimbursement pressure.
Operational Changes Beyond Payment Adjustments
The final rule introduces several operational modifications that agencies must implement by January 1, 2026. CMS updated the face-to-face encounter policy to allow any physician to perform encounters regardless of whether they are the certifying practitioner or previously cared for the patient in the referring facility. This change provides agencies with greater flexibility in meeting documentation requirements.

The agency also recalibrated Patient-Driven Groupings Model case weights and low-utilization payment adjustment (LUPA) thresholds using 2024 data. This recalibration aims to better reflect current patient populations and utilization patterns, potentially creating opportunities for agencies with specific case mixes to optimize their revenue.
Quality Measures and Value-Based Care Implications
The Home Health Value-Based Purchasing (HHVBP) model underwent significant modifications in the final rule. CMS removed three CAHPS-based measures while adding four new measures, including the claims-based Medicare Spending per Beneficiary for Post-Acute Care measure and three OASIS-based self-care functional measures focused on bathing and dressing.
These changes align with broader industry trends toward value-based care models that prioritize patient outcomes and cost efficiency. As we discussed in our comprehensive analysis of value-based versus fee-for-service models, agencies that excel in quality metrics and care coordination are better positioned to thrive under evolving reimbursement structures.
The emphasis on functional outcome measures reflects CMS's focus on meaningful patient improvements rather than process metrics alone. Agencies should evaluate how their current care protocols and documentation practices align with these new quality indicators.
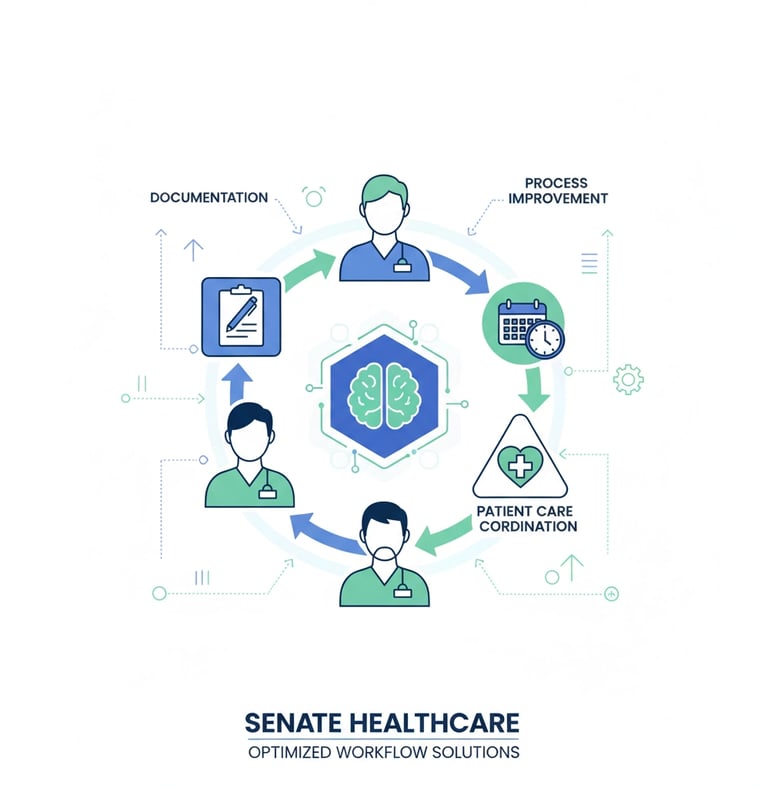
Strategic Response Framework for Agency Leaders
Immediate Financial Assessment
Agency owners should conduct an immediate financial impact analysis based on their specific patient mix and service volume. The $19 per 30-day period average reduction will vary significantly depending on case complexity and geographic factors. Understanding your agency's specific exposure enables more targeted operational adjustments.
Review your current Patient-Driven Groupings Model case weight distribution against the recalibrated categories. Some agencies may find opportunities to optimize case mix or adjust service delivery models to work more effectively within the updated payment framework.
Operational Efficiency Optimization
The updated face-to-face encounter policy creates opportunities for operational streamlining. Agencies can now utilize physician relationships more flexibly, potentially reducing administrative burden and improving workflow efficiency. Consider how this change might allow for better resource allocation or improved physician engagement strategies.


Evaluate your current documentation and quality reporting systems against the new HHVBP measures. Agencies with robust data collection and analysis capabilities will be better positioned to excel under the updated quality framework and potentially offset payment reductions through performance bonuses.
Long-Term Strategic Positioning
The sustained pattern of Medicare payment reductions signals a need for fundamental strategic reassessment. As we explored in our analysis of succession planning as a strategic advantage, agencies must consider whether their current operational model remains viable long-term or whether strategic alternatives merit consideration.
This includes evaluating potential partnerships, service line diversification, or exit strategies. The current reimbursement environment favors larger, more efficient operations that can leverage economies of scale and advanced technology platforms.
Technology and Innovation Opportunities
Agencies should accelerate adoption of technology solutions that improve care efficiency and quality outcomes. This includes telehealth integration, remote patient monitoring, and data analytics platforms that support the new quality measures. Our analysis of telehealth and personalized care strategies provides guidance on implementing these technologies effectively.
The emphasis on functional outcome measures creates opportunities for agencies that invest in comprehensive care planning and patient engagement tools. These investments may initially impact margins but can position agencies for better performance under value-based purchasing models.
Preparing for Implementation
With the January 1, 2026 implementation date approaching, agencies must prioritize preparation activities. This includes staff training on updated documentation requirements, system updates to accommodate new quality measures, and financial planning to manage the payment reduction impact.
Consider conducting scenario planning exercises to evaluate how different patient volume or case mix changes might affect your agency's financial performance under the new payment structure. This preparation enables more proactive management as the rule takes effect.
The 2026 Home Health Medicare Payment Rule represents a significant improvement over the originally proposed cuts while maintaining pressure on agencies to operate more efficiently. Success will require strategic thinking, operational excellence, and careful attention to quality metrics that increasingly drive reimbursement outcomes.
Resources:
CMS Fact Sheet: Calendar Year (CY) 2026 Home Health Prospective Payment System Final Rule (CMS-1828-F)
https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2026-home-health-prospective-payment-system-final-rule-cms-1828-fHome Health Care News: CMS Finalizes 2026 Home Health Medicare Payment Rule With 1.3% Aggregate Reduction
https://homehealthcarenews.com/2025/11/cms-finalizes-2026-home-health-medicare-payment-rule-with-1-3-aggregate-reduction/Home Health Care News (related historical context): Congress Must Intervene: Home Health Leaders React To Third Consecutive Year Of Payment Cuts
https://homehealthcarenews.com/2024/11/congress-must-intervene-home-health-leaders-react-to-third-consecutive-year-of-payment-cuts/CMS: Expanded Home Health Value-Based Purchasing Model
https://www.cms.gov/priorities/innovation/innovation-models/expanded-home-health-value-based-purchasing-modelNet Health: Fee-for-Service vs Value-Based Care: What’s the Difference?
https://www.nethealth.com/blog/fee-for-service-vs-value-based-care-what-difference/American Hospital Association: CMS Proposes 6.4% Decrease to Home Health Payments for CY 2026, Updates Quality and Value-Based Purchasing
https://www.aha.org/news/headline/2025-06-30-cms-proposes-64-decrease-home-health-payments-cy-2026-updates-quality-and-value-based-purchasing
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED