Telehealth & Personalized Care: Core Strategies for Competitive Home Health Agencies in 2025
This blog post examines how telehealth integration and personalized care planning have become essential competitive strategies for home health agencies in 2025, covering implementation approaches, policy challenges, and market opportunities.
11/13/20256 min read


The Strategic Imperative for Telehealth Integration
Home health agencies in 2025 face unprecedented pressure to adopt technology-driven care models. The convergence of workforce shortages, evolving patient expectations, and regulatory changes has transformed telehealth from an optional service to a core competitive requirement.
Recent industry surveys reveal that 53% of home health agencies identify remote patient monitoring as a key strategic priority, while 49% prioritize telehealth and virtual visits. This broad consensus reflects recognition that these capabilities directly correlate with operational efficiency and market positioning.


Multi-Modal Telehealth Deployment
Competitive agencies are moving beyond basic video calls to implement comprehensive telehealth ecosystems. Successful deployment involves three primary modalities:
Tele-video consultations enable real-time visual assessments and complex care coordination between patients, caregivers, and specialists. These sessions prove particularly valuable for wound care monitoring, medication management reviews, and family education sessions.
Tele-calls provide cost-effective check-ins for routine monitoring, appointment scheduling, and basic health status updates. This approach works especially well for patients with stable chronic conditions who need regular but less intensive oversight.
Remote monitoring systems collect continuous health data through wearable devices and home-based sensors. These systems track vital signs, medication adherence, and activity levels, enabling proactive interventions before conditions deteriorate.
The strategic advantage lies not in choosing one modality but in creating integrated platforms where different telehealth approaches work together seamlessly. Leading agencies use this integration to optimize resource allocation, ensuring that high-skill clinicians focus on complex cases while routine monitoring happens virtually.
Hybrid Care Models as Market Differentiators
The most successful agencies in 2025 have abandoned the false choice between virtual and in-person care, instead developing sophisticated hybrid models that strategically combine both approaches.


Optimizing Visit Allocation
Hybrid care models enable agencies to allocate their most expensive resource, skilled nursing time, more strategically. Virtual check-ins reduce unnecessary in-home visits, conserving staff capacity for patients who truly need hands-on intervention. This approach proves particularly valuable for chronic disease management, where continuous monitoring through virtual follow-ups improves medication adherence and clinical outcomes while reducing emergency room visits.
For example, a diabetes management program might include weekly virtual consultations for blood sugar review and medication adjustments, combined with monthly in-person visits for comprehensive health assessments and equipment maintenance. This balance maintains clinical quality while improving operational efficiency.
Geographic Expansion Through Technology
Telehealth capabilities allow agencies to serve patients beyond their traditional geographic boundaries. Rural and transportation-limited populations particularly benefit from virtual care alternatives, creating new market opportunities for agencies willing to invest in robust telehealth infrastructure.
Personalized Care Planning as Premium Positioning
The transition from standardized care protocols to truly personalized care plans represents one of the most significant competitive opportunities in 2025. Agencies implementing data-driven customization position themselves as premium service providers in an increasingly commoditized market.


Data-Driven Customization
Personalized care planning relies on comprehensive health assessments that inform disease-focused strategies tailored to individual medical histories, lifestyle factors, and personal preferences. Technology integration facilitates this customization by aggregating data from multiple sources including electronic health records, remote monitoring devices, and patient-reported outcomes.
The most advanced agencies use artificial intelligence to identify patterns in patient data that inform care plan adjustments. For instance, if remote monitoring reveals that a patient's symptoms consistently worsen during specific weather patterns or at particular times of day, care plans can be proactively adjusted to provide additional support during these high-risk periods.
Patient Loyalty Through Customization
Personalized care creates significant competitive moats through improved patient satisfaction and loyalty. Patients receiving truly customized care plans demonstrate higher satisfaction scores and reduced likelihood of switching providers. This loyalty becomes increasingly valuable as patient choice expands and competition intensifies.
Navigating the Policy Landscape
The regulatory environment for telehealth continues evolving, creating both opportunities and challenges for home health agencies. Understanding and adapting to these changes remains critical for strategic success.
Post-Pandemic Policy Adjustments
Telehealth adoption accelerated dramatically during the pandemic, growing from 23% of home health agencies in 2019 to a peak of 65%. However, this growth masks concerning discontinuation trends, with 19% of agencies that adopted telehealth during the pandemic having discontinued services by 2024.
Key factors driving discontinuation include reimbursement uncertainty, regulatory complexity, and technology integration challenges. Agencies that successfully navigate these obstacles gain significant competitive advantages as competitors retreat from telehealth services.
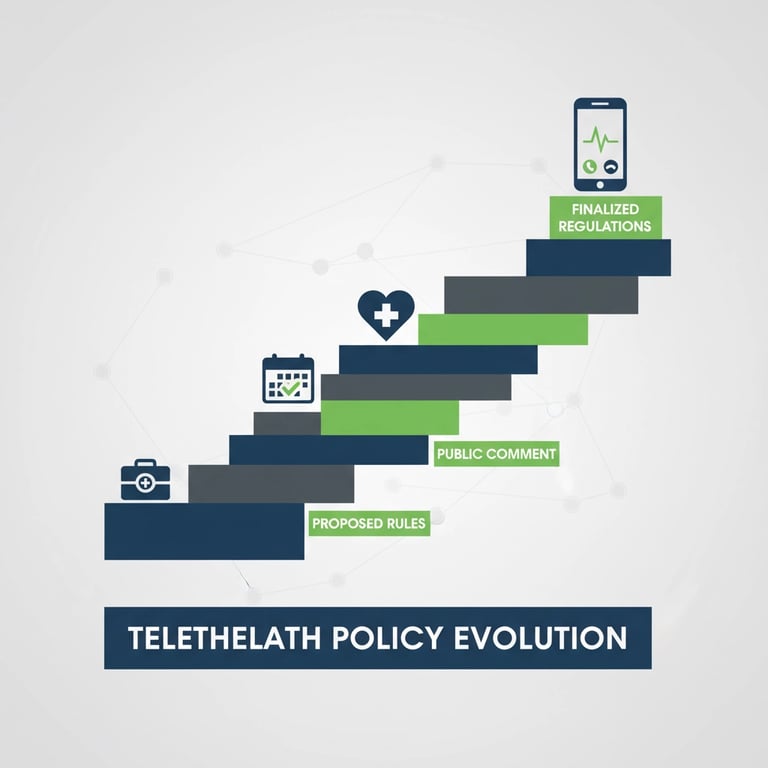

Critical Policy Transitions
Recent policy changes have created both challenges and opportunities. While some pandemic-era flexibilities have expired, new capabilities have emerged. Physicians and practitioners can now use two-way, real-time audio-only communication technology for telehealth services, expanding access options for patients with limited video capabilities.
Agencies serving rural and underserved populations must pay particular attention to policy developments, as these communities depend most heavily on telehealth alternatives for accessing care.
Workforce Development Through Technology
Telehealth expansion enables innovative workforce strategies that address critical staffing challenges. Virtual supervision of clinical staff across geographic boundaries allows agencies to centralize oversight functions while distributing service delivery more broadly.
Expanding Recruitment Reach
Remote supervision capabilities permit agencies to recruit skilled clinicians from beyond local labor markets. A agency based in one state can employ and supervise nurses or therapists located hundreds of miles away, dramatically expanding the potential workforce pool.
This geographic flexibility proves especially valuable for specialized services where qualified professionals may be concentrated in specific regions. For example, an agency might employ a wound care specialist located in an urban medical center to provide virtual consultations for patients across multiple rural service areas.
Technology Integration Best Practices
Successful telehealth implementation requires careful attention to technology selection and integration processes. The most effective agencies focus on platforms that integrate seamlessly with existing electronic health records and billing systems.


Platform Selection Criteria
Leading agencies evaluate telehealth platforms based on several critical factors:
Interoperability with existing clinical and administrative systems reduces duplicate data entry and improves workflow efficiency.
Scalability ensures that technology investments can grow with the agency without requiring complete system replacements.
User experience for both clinicians and patients affects adoption rates and long-term success.
Compliance capabilities help ensure adherence to HIPAA and other regulatory requirements.
Implementation Strategy
Successful telehealth implementation follows phased approaches that allow agencies to learn and adjust before full-scale deployment. Pilot programs with specific patient populations or service lines help identify potential challenges and refine processes before broader implementation.
Market Opportunities and Growth Potential
The home healthcare market continues expanding substantially, creating significant opportunities for agencies that successfully integrate telehealth and personalized care capabilities. Market analysis projects growth from $305.4 billion in 2025 to $551.1 billion by 2032.
This expansion reflects aging population demographics, increasing preference for aging in place, and growing recognition of home-based care's cost-effectiveness compared to institutional alternatives.
Competitive Positioning
Agencies that view telehealth and personalization as integrated components of comprehensive competitive strategy, rather than isolated initiatives, capture disproportionate market share in this expanding sector. The combination of robust telehealth infrastructure with truly personalized care plans, supported by sophisticated workforce management, creates sustainable operational advantages that competitors find difficult to replicate.
Success in 2025 and beyond belongs to agencies that embrace technology not as a replacement for human care but as an enhancement that enables more personalized, efficient, and effective service delivery. The integration of telehealth capabilities with genuinely customized care planning represents the new standard for competitive home health operations.
For agencies looking to develop comprehensive strategies around these opportunities, partnering with experienced healthcare advisory firms can accelerate implementation while avoiding common pitfalls that have led other providers to discontinue their telehealth initiatives.
Sources:
https://www.aha.org/fact-sheets/2025-02-07-fact-sheet-2025-telehealth-advocacy-agenda
https://caretap.net/blog/strategies-home-care-providers-jumpstart-growth/
https://synchronyfl.com/the-future-of-home-health-care-trends-to-watch-in-2025/
https://axiscare.com/white-papers/access-home-care-industry-survey-and-trends-report/
https://www.cms.gov/files/document/telehealth-faq-updated-10-15-2025.pdf
https://engage.axxess.com/rs/437-WGW-363/images/2025_Trends_Report__Final-Web.pdf?version=0
https://www.ama-assn.org/health-care-advocacy/advocacy-update/nov-7-2025-national-advocacy-update
https://telehealth.hhs.gov/providers/telehealth-policy/telehealth-policy-updates
https://www.coherentmarketinsights.com/industry-reports/home-health-care-agency-market
https://www.chcs.org/resource-center/telehealth-in-complex-care/
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED