Value-Based Care vs Fee-for-Service: Which Reimbursement Model Will Save Your Home Health Agency in 2026?
This comprehensive analysis examines fee-for-service versus value-based care reimbursement models for home health agencies facing 2026's challenging payment landscape. We explore the pros and cons of each approach, analyze the critical 2026 regulatory changes, and provide strategic recommendations for agency owners navigating Medicare payment cuts while positioning for long-term sustainability. The piece includes detailed comparisons and practical implementation guidance for agencies considering value-based care transitions.
11/27/20255 min read


The 2026 reimbursement landscape is forcing home health agencies to make critical decisions about their payment models that could determine their survival. With Medicare proposing significant payment cuts and CMS doubling down on value-based initiatives, agency owners need clarity on which approach offers the best path forward.
The Stakes Have Never Been Higher
Home health agencies are facing a perfect storm in 2026. CMS has proposed a 6.4% decrease to home health payments, translating to approximately $1.135 billion in reduced Medicare reimbursement compared to 2025. At the same time, the agency is expanding value-based purchasing programs and emphasizing alternative payment models that reward quality over quantity.
This isn't just about surviving another round of cuts. It's about positioning your agency for long-term sustainability in a healthcare system that's fundamentally shifting away from volume-based reimbursement.


Fee-for-Service: The Traditional Path
Fee-for-service has been the backbone of home health reimbursement for decades. Under this model, agencies receive payment for each individual service delivered, regardless of patient outcomes or care coordination.
The FFS Advantages
Fee-for-service offers several practical benefits that explain its enduring popularity. The infrastructure is well-established, with familiar billing processes and predictable revenue streams based on service volume. Providers maintain significant autonomy in treatment decisions, and patients enjoy broad choice in selecting their care providers.
For agencies with efficient operations, FFS can provide steady cash flow. You know exactly what each visit, therapy session, or skilled nursing service will generate in revenue. This predictability makes financial planning and staffing decisions more straightforward.
The FFS Challenges
However, the fee-for-service model creates perverse incentives that are increasingly problematic. Because reimbursement is tied to service volume, agencies have financial incentives to provide more services, even when they may not be clinically necessary. This can lead to overutilization and higher overall healthcare costs.
More critically, FFS discourages care coordination. Since agencies aren't financially rewarded for collaborating with other providers or focusing on preventive care, patients often experience fragmented care with poor communication between providers.
Value-Based Care: The Future-Focused Alternative
Value-based care flips the traditional model by reimbursing providers based on the quality of care and outcomes achieved, not the volume of services delivered. For home health agencies, this primarily manifests through the Home Health Value-Based Purchasing (HHVBP) Model and various shared savings programs.


How Value-Based Models Work
Under value-based arrangements, agencies can participate in several types of programs:
Capitation arrangements where you receive a fixed payment per patient per period
Bundled payments covering all services for treating specific conditions
Shared savings programs where agencies earn bonuses for meeting cost and quality targets
The HHVBP Model which adjusts payments based on performance against quality measures
The expanded HHVBP Model launching in 2026 includes four new quality measures focusing on Medicare spending per beneficiary and functional improvement outcomes. Agencies that perform well can earn significant bonuses, while poor performers may face payment reductions.
The Value-Based Advantages
Early results from value-based programs are encouraging. The original HHVBP Model achieved an average 4.6% improvement in total performance scores and generated average annual Medicare savings of $141 million. Participating agencies also demonstrated reduced unplanned hospitalizations and skilled nursing facility stays.
Value-based care incentivizes the coordination and preventive focus that leads to better patient outcomes. When your revenue depends on keeping patients healthy and out of the hospital, you naturally invest in comprehensive care planning and proactive management.
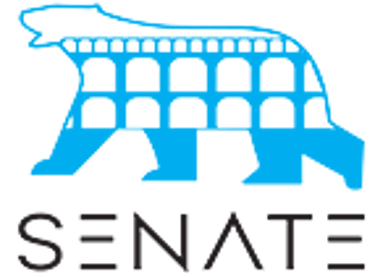
The Critical Comparison


2026: The Tipping Point
The 2026 regulatory environment makes clear that CMS is accelerating the shift toward value-based care. The proposed Medicare Physician Fee Schedule rule explicitly emphasizes value-based care, efficiency adjustments, and alternative payment models.
For home health specifically, agencies face a challenging math problem. The proposed 6.4% payment reduction affects all FFS reimbursement, but agencies participating in value-based programs can potentially offset these cuts through performance bonuses and shared savings.
Consider the math: if your agency generates $5 million annually in Medicare revenue, a 6.4% cut costs you $320,000. However, high-performing agencies in the HHVBP Model can earn bonuses that potentially offset much of this reduction.
Strategic Recommendations for Agency Owners
For Most Agencies: A Hybrid Approach
The optimal strategy for 2026 combines both models strategically. Continue optimizing your FFS operations while gradually building value-based capabilities. This allows you to maintain current revenue while positioning for future opportunities.
Start by maximizing participation in available value-based programs, particularly the expanded HHVBP Model. Even modest improvements in quality scores can generate meaningful bonus payments that help offset FFS cuts.
Investment Priorities
Successful value-based participation requires specific infrastructure investments:
Care coordination systems that track patient progress across episodes
Data analytics capabilities to identify high-risk patients and intervention opportunities
Staff training on population health management and preventive care protocols
Quality measurement and reporting systems for tracking performance metrics
These investments pay dividends beyond value-based programs. Better care coordination and outcome tracking improve patient satisfaction and referral relationships, benefiting your overall business.


Timeline Considerations
Agencies should view 2026 as a transition year rather than a final destination. The regulatory momentum clearly favors value-based models, and future payment cuts to FFS are likely. Agencies that begin building value-based capabilities now avoid disruptive transitions later.
For agencies considering strategic partnerships or transitions, value-based experience significantly enhances acquisition value. Buyers prize agencies with demonstrated value-based capabilities and established quality metrics.
The Bottom Line
Value-based care offers superior long-term positioning for home health agencies, but the transition requires careful planning and investment. The agencies that will thrive beyond 2026 are those that view value-based care not as a threat to their FFS revenue, but as an essential complement that generates incremental savings-based revenue while improving financial sustainability.
The 2026 payment cuts and regulatory emphasis on value-based models create urgency around this decision. Agencies that continue operating purely under fee-for-service will face declining margins and increasing regulatory pressure. Those that begin building value-based capabilities now position themselves for sustainable growth in the evolving healthcare landscape.
For agency owners evaluating their options, the question isn't whether to embrace value-based care, but how quickly and strategically to make the transition while maintaining operational stability and financial performance.
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED