Stop Losing Revenue to Telehealth Confusion: The Proven Framework to Maximize Hospital-at-Home Opportunities
This comprehensive guide reveals how home health agencies can stop losing revenue to telehealth confusion by implementing a proven framework for hospital-at-home opportunities. Learn the specific technical infrastructure requirements, service delivery models, and regulatory strategies that successful agencies use to maximize ROI while improving patient outcomes. Discover how to overcome common implementation barriers and build sustainable competitive advantages in the rapidly evolving healthcare landscape.
11/24/20255 min read


Home health agencies are leaving millions on the table due to telehealth confusion and missed hospital-at-home opportunities. This post reveals the proven framework that successful agencies use to maximize revenue from these rapidly expanding programs while navigating regulatory complexities.
The Revenue Confusion Crisis
Most home health agencies recognize that telehealth and hospital-at-home programs represent significant growth opportunities, yet many struggle with implementation and revenue optimization. The confusion stems from rapidly evolving regulations, unclear reimbursement models, and the challenge of integrating new technology with existing care delivery systems.
The stakes are high. Recent regulatory updates show that agencies who successfully leverage these programs can see dramatic improvements in both patient outcomes and financial performance. Conversely, agencies that fail to adapt risk losing market share to more technologically savvy competitors.

Understanding the True Revenue Potential
Hospital-at-home and telehealth programs generate revenue through multiple mechanisms that many agencies overlook. The core strategy involves increased patient access and capacity, allowing providers to see more patients while reducing operational overhead. When agencies implement these services effectively, administrative tasks move online, enabling clinicians to spend more time delivering billable care rather than performing non-revenue generating activities.
The financial impact extends beyond direct patient care revenue. These programs help agencies avoid costly patient transfers and emergency department visits. For every patient kept at home rather than transferred to higher levels of care, agencies can preserve substantial revenue while improving patient satisfaction scores.
Cost reduction occurs through several pathways:
Automation of routine tasks decreases administrative staffing requirements
Reduced travel time allows for higher patient visit volumes
Improved care coordination reduces duplicate services
Enhanced monitoring prevents costly readmissions
Early adopters of comprehensive telehealth programs have experienced significant increases across all revenue categories. One documented example shows savings of $5.6 million through reduced inpatient stays and improved care coordination.
The Proven Revenue Maximization Framework
Technical Infrastructure Foundation
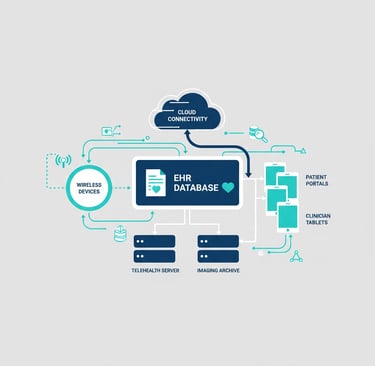
Successful agencies build their hospital-at-home programs on robust technical systems. This includes scalable models utilizing biometrically enhanced video conferencing, wireless devices for vital sign collection, and integrated electronic health records (EHR). However, many agencies face barriers in maximizing their EHR potential.
The solution involves platforms that ingest existing EHR data and convert it into personalized clinical decision support tools. These systems must comply with local privacy rules while providing real-time insights for informed clinical management.

Service Delivery Model Structure
Effective programs establish clear care period structures. Successful models typically include defined timeframes that encompass acute care at home followed by extended post-acute monitoring. This circumscribed timeline provides clarity for revenue coding and operational planning while ensuring continuity of care.
The key is creating standardized protocols that align with existing telehealth and personalized care strategies. Rather than creating entirely new systems, hospital-at-home programs should integrate with current care delivery models, including post-discharge follow-up protocols.
Quality and Access Standardization
National measurement frameworks identify four critical domains for evaluation: access to care, financial impact and cost, patient experience, and clinical effectiveness. When providers see patients more frequently through telehealth, their knowledge of patient situations increases, enabling more personalized and efficient care delivery.
Research confirms that both providers and patients report no noticeable difference in virtual visit quality compared to in-person visits when proper protocols are followed. This quality maintenance while reducing costs creates the optimal scenario for revenue growth.
Overcoming Revenue Cannibalization Concerns
Many agencies worry that telehealth will cannibalize traditional in-person fee-for-service models. This concern is misplaced. The reality is that traditional models alone cannot sustain modern healthcare agencies facing ongoing reimbursement challenges.
Instead, telehealth serves as a complementary strategy that increases total revenue while reducing per-visit costs. This creates higher bottom-line margins without sacrificing care quality. The key is proper implementation that enhances rather than replaces existing services.


Current Regulatory Opportunities
The regulatory landscape presents unprecedented opportunities for agencies willing to act quickly. Medicare telehealth flexibilities and the Acute Hospital Care at Home program have been extended through January 2026, with retroactive payment provisions for services previously under temporary waivers.
Recent policy changes have permanently eliminated several barriers:
Virtual direct supervision of clinical staff is now permanently allowed
Frequency limits on subsequent visits have been eliminated
Critical care consultations via telehealth are fully reimbursable
These permanent policy changes eliminate previous uncertainty about reimbursement and provide the regulatory stability needed for long-term program investment.
As of mid-2025, over 400 hospitals across 39 states have been approved to provide hospital-at-home services, demonstrating widespread adoption and establishing proven operational models that home health agencies can adapt.
Implementation Priorities for Maximum ROI
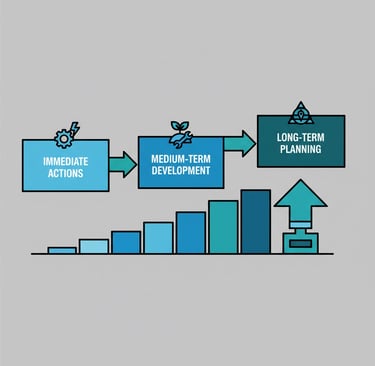
To maximize hospital-at-home opportunities and eliminate revenue confusion, agencies should prioritize specific implementation steps:
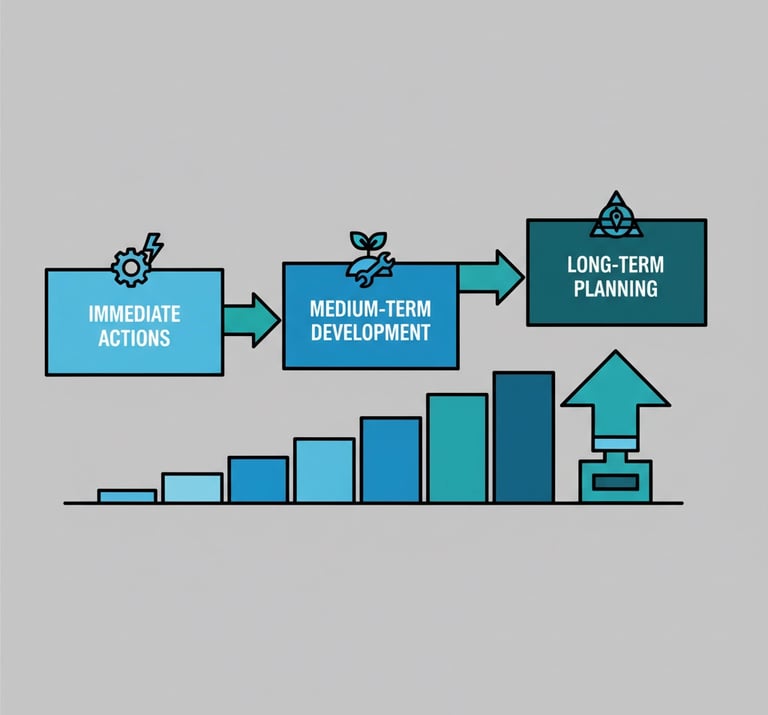
Immediate Actions:
Establish clear technical infrastructure with EHR integration
Align programs with existing post-discharge protocols
Train staff on permanent regulatory flexibilities
Identify patient populations most likely to benefit
Medium-term Development:
Implement comprehensive outcome measurement across all four evaluation domains
Develop partnerships with local hospitals and health systems
Create standardized care protocols for common conditions
Build quality reporting systems for payer negotiations
Long-term Strategic Planning:
Integrate hospital-at-home capabilities into succession planning strategies
Develop competitive advantages through technology differentiation
Build scalable systems for geographic expansion
Measuring Success and Scaling Programs
Successful agencies implement comprehensive measurement systems that track both clinical and financial outcomes. Key performance indicators should include patient satisfaction scores, readmission rates, cost per episode, and revenue per patient.
The most successful programs treat hospital-at-home services as permanent components of their care delivery system rather than temporary measures. This long-term perspective enables agencies to build sustainable competitive advantages while improving patient access and financial performance.
Financial tracking should focus on total cost of care rather than individual visit reimbursement. This broader view reveals the true value proposition of preventing expensive hospitalizations and emergency department visits through proactive home-based care.
Building Competitive Advantage
Agencies that successfully implement comprehensive hospital-at-home programs create significant competitive moats. These advantages compound over time as technology systems improve and clinical protocols become more refined.
The current market presents a window of opportunity for agencies willing to invest in these capabilities before they become standard expectations. Early movers can capture market share and establish referral relationships that become difficult for competitors to replicate.
For agencies considering strategic partnerships or exits, strong telehealth and hospital-at-home capabilities significantly increase valuation multiples. Acquirers and partners actively seek agencies with demonstrated technology competencies and diversified service offerings.
The path forward requires commitment to both technology investment and cultural change within the organization. However, agencies that successfully navigate this transition position themselves for sustained growth in an increasingly competitive healthcare landscape.
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED