Federal Funding Chaos: 7 Mistakes You're Making with Medicare Budget Prep (and How to Fix Them Before 2026)
Medicare funding uncertainty and CMS payment rule changes are creating unprecedented budgeting challenges for home health, home care, and hospice agencies approaching 2026. This comprehensive guide identifies seven critical budget preparation mistakes that could cost agencies thousands in lost revenue and reduced valuations, while providing actionable solutions to build financial resilience. Agency owners considering exit strategies or growth partnerships will find essential insights for maintaining competitive positioning and maximizing deal potential during industry turbulence.
12/19/20255 min read
Medicare funding uncertainty and regulatory changes are creating unprecedented challenges for home health, home care, and hospice agencies heading into 2026. With CMS finalizing significant payment rule changes and Congress considering substantial Medicare cuts, agencies that fail to prepare their budgets properly risk operational disruption, reduced valuations, and potential buyer hesitation during M&A transactions.
The Stakes Have Never Been Higher
The healthcare landscape is shifting rapidly. CMS has finalized the FY 2026 hospice payment rule with meaningful updates to reimbursement structures, while Congress continues to debate Medicare cuts that could reach up to 9% across various programs. For agency owners considering exit strategies or partnerships, these budgeting mistakes can directly impact deal multiples and buyer confidence.
Home health agencies face their biggest test yet with proposed 2026 Medicare payment cuts threatening industry stability. Meanwhile, regulatory compliance costs continue to climb, and the competitive landscape intensifies as private equity and strategic buyers become increasingly selective about acquisition targets.
Mistake #1: Underestimating CMS Reimbursement Rate Volatility
Many agencies budget based on current reimbursement rates without adequately modeling potential decreases. The FY 2026 hospice payment rule includes updates that will affect agency revenue streams, yet too many operators use static projections that ignore regulatory volatility.
The Financial Risk: A 3-5% reimbursement reduction can eliminate 20-30% of an agency's EBITDA, directly impacting valuation multiples during potential sales.


How to Fix It: Develop scenario-based budget models with conservative, moderate, and optimistic reimbursement assumptions. Build cash reserves equal to 3-6 months of operating expenses specifically for regulatory adjustment periods. Track CMS payment rule changes quarterly and adjust projections accordingly.
Buyer Impact: Sophisticated buyers now require agencies to demonstrate financial resilience through multiple reimbursement scenarios. Agencies with robust scenario planning command higher multiples because they present lower operational risk.
Mistake #2: Failing to Account for Escalating Compliance Costs
Regulatory compliance expenses continue to climb, yet many agencies budget these costs as static line items rather than growing operational requirements. New documentation standards, quality reporting obligations, and audit preparation costs are consuming increasing percentages of agency resources.
The Hidden Drain: Compliance costs can grow 15-25% annually, often hidden across payroll, technology, and administrative expenses rather than tracked as a dedicated budget category.
How to Fix It: Create a dedicated compliance budget category that includes staff training, technology upgrades, documentation systems, and external consulting. Plan for 20-25% annual increases in compliance-related expenses through 2026. Implement compliance tracking systems that provide real-time cost visibility.
Strategic Advantage: Agencies with sophisticated compliance infrastructure often become acquisition targets because buyers value operational readiness and reduced regulatory risk.
Mistake #3: Ignoring Patient Population Demographics and Payer Mix Shifts
Medicare Advantage growth continues to accelerate, changing the fundamental economics of patient care. Agencies that budget based on traditional Medicare reimbursement patterns without accounting for MA plan negotiations and requirements face significant revenue surprises.
The Shift: Medicare Advantage enrollment has grown consistently, with different authorization requirements, network restrictions, and reimbursement structures compared to traditional Medicare.
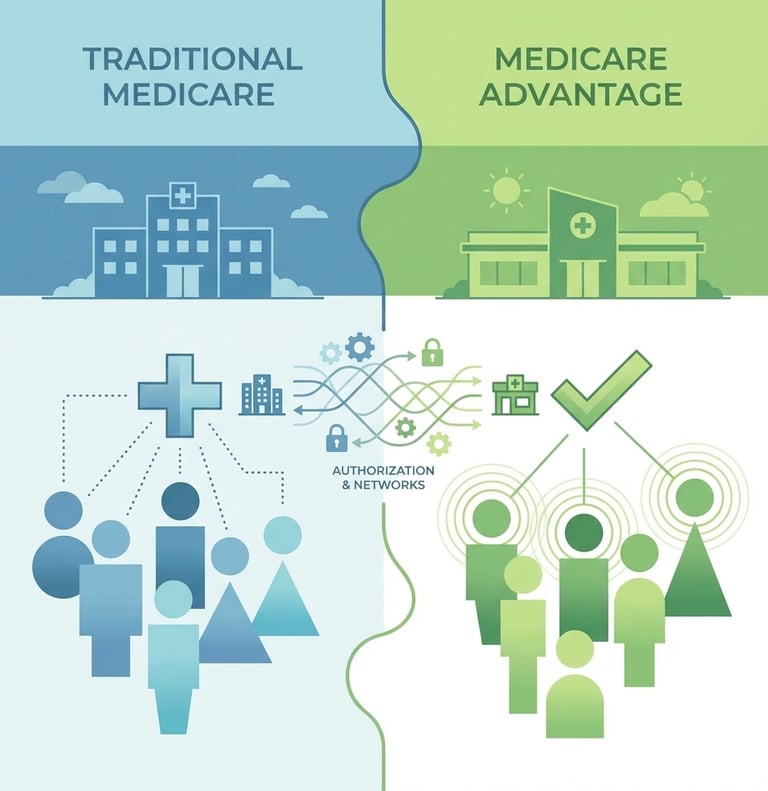
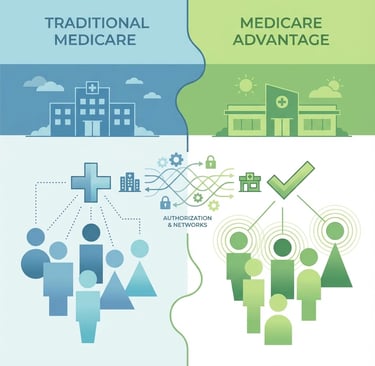
How to Fix It: Analyze your current payer mix trends and project MA growth impact on your patient population. Develop separate budget models for traditional Medicare versus Medicare Advantage patients. Build relationships with major MA plans in your market to understand future contract terms.
M&A Consideration: Buyers increasingly prefer agencies with diversified payer relationships and demonstrated success managing Medicare Advantage contracts. Strong MA relationships can add 10-15% to agency valuations.
Mistake #4: Overlooking Technology Infrastructure Investment Requirements
Regulatory reporting, quality measures, and operational efficiency increasingly depend on sophisticated technology platforms. Agencies that treat technology as a discretionary expense rather than essential infrastructure face compliance gaps and competitive disadvantages.
The Investment Reality: Effective EMR systems, patient monitoring platforms, and compliance software require significant upfront investment plus ongoing subscription costs that many agencies underestimate.
How to Fix It: Budget 8-12% of gross revenue for technology infrastructure, including software subscriptions, hardware updates, staff training, and system integration costs. Evaluate technology needs annually rather than reactively addressing problems.
Valuation Impact: Technology-forward agencies command premium valuations because buyers recognize reduced operational risk and scalability potential. Modern tech infrastructure can add 20-30% to deal multiples.
Mistake #5: Inadequate Cash Flow Management During Regulatory Transition Periods
Medicare payment timing, claim processing delays, and audit-related cash flow interruptions can create serious liquidity challenges. Agencies that maintain minimal cash reserves or credit facilities often struggle during regulatory adjustment periods.
The Cash Crunch: CMS payment delays can extend 60-90 days during system updates or audit periods, while agencies must maintain full operations and payroll obligations.


How to Fix It: Maintain operating credit lines equal to 90-120 days of expenses. Establish relationships with healthcare-focused lenders who understand industry cash flow patterns. Implement daily cash flow monitoring with 13-week rolling projections.
Exit Readiness: Strong cash management demonstrates operational sophistication to potential buyers. Agencies with robust financial controls and cash management systems complete M&A transactions more smoothly and at higher valuations.
Mistake #6: Missing Documentation and Quality Reporting Updates
CMS continuously updates documentation requirements and quality reporting standards. Agencies that fail to budget for these evolving requirements face audit penalties, reimbursement clawbacks, and potential exclusion from Medicare programs.
The Compliance Trap: Documentation requirements often change with minimal notice, requiring immediate staff retraining and system updates that can cost $50,000-$150,000 per implementation cycle.
How to Fix It: Allocate 3-5% of annual revenue specifically for documentation and quality initiative compliance. Subscribe to CMS updates and industry intelligence services. Train administrative staff to monitor regulatory changes and assess budget impact.
Risk Mitigation: Buyers conduct extensive compliance due diligence. Agencies with documented compliance tracking and proactive update management reduce buyer concerns about hidden regulatory liabilities.
Mistake #7: Not Preparing for Competitive Landscape Evolution
The healthcare services market continues consolidating as larger operators acquire smaller agencies and private equity increases industry involvement. Agencies that budget in isolation without considering competitive pressures often find themselves at strategic disadvantages.
The Market Reality: Competition for quality staff, patient referrals, and strategic partnerships intensifies annually. Agencies must budget for competitive wages, enhanced service offerings, and strategic positioning initiatives.
How to Fix It: Research competitor compensation structures and service offerings annually. Budget for market-rate wages plus 10-15% premium for critical positions. Allocate resources for service line expansion and strategic partnership development.
Strategic Positioning: Well-positioned agencies become acquisition targets rather than acquisition casualties. Strategic budget allocation for competitive positioning can result in premium exit valuations when owners decide to sell.
Building Financial Resilience for 2026 and Beyond
Successful agencies approach Medicare budget preparation as strategic planning rather than accounting exercises. They model multiple scenarios, maintain adequate reserves, and invest in infrastructure that supports sustainable growth regardless of regulatory changes.
The most successful agency owners recognize that proper budget preparation directly impacts exit readiness and valuation potential. Whether planning for organic growth, strategic partnerships, or eventual sale, financial resilience through sophisticated budgeting creates options and maximizes outcomes.
For agencies considering succession planning or M&A opportunities, demonstrating financial sophistication through comprehensive budget preparation becomes a competitive advantage. Buyers pay premiums for agencies that prove operational resilience and strategic thinking through their financial management practices.
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED