The Ultimate Guide to Surviving CMS Rate Cuts: Everything You Need to Succeed in 2026
A comprehensive survival guide for home health and hospice agencies facing CMS rate cuts in 2026. This actionable resource covers the 6.4% payment reduction impact, provides a 90-day implementation strategy, and offers proven revenue optimization techniques to help healthcare organizations thrive despite challenging reimbursement changes.
9/22/20254 min read
The healthcare landscape is about to get rougher. CMS has proposed a staggering 6.4% decrease in home health payments for 2026, representing a 1.13 billion dollar industry-wide reduction. While Medicare Advantage plans will see increases, home health agencies face their biggest financial challenge in years.
Here's the reality: half of U.S. counties have already lost home health agencies, and 70% are treating fewer Medicare patients. But this isn't a death sentence. It's a wake-up call for agencies ready to adapt, optimize, and thrive.
Understanding the 2026 Rate Cut Structure
The 6.4% reduction isn't just one simple cut. According to CMS's proposed rule, it breaks down into several components:
3.2% market basket update reduced by 0.8% productivity adjustment
4.1% permanent reduction to prevent future overpayments
5.0% temporary reduction to recoup past overpayments
0.5% reduction for high-cost outlier payments
This layered approach means agencies can't simply absorb the cuts through minor operational tweaks. You need a comprehensive survival strategy.


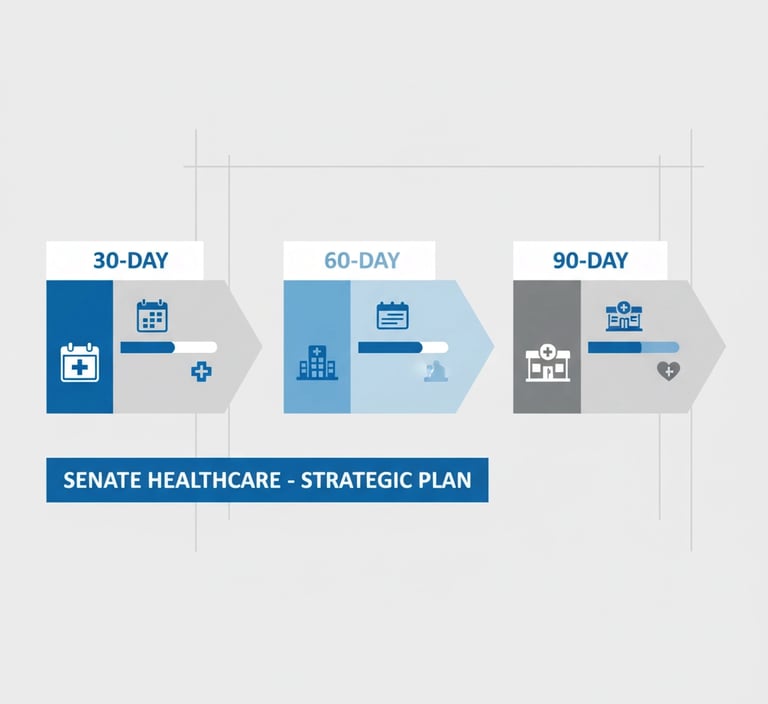
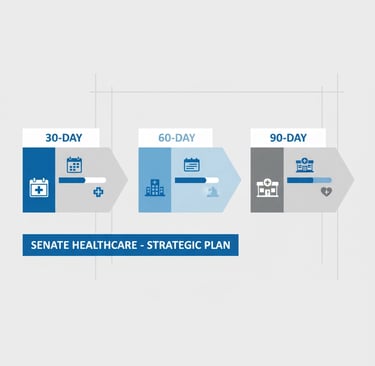
The 90-Day Emergency Action Plan
Days 1-30: Financial Reality Check
Start with brutal honesty about your financial position. Calculate your true margin per Patient-Driven Groupings Model (PDGM) period, not just overall agency margins. Key metrics to analyze immediately:
Payer mix percentage and profitability by payer
Days sales outstanding (DSO)
Days cash on hand
Administrative cost percentage
OASIS accuracy rates
Conduct a comprehensive coding audit. Every documentation error costs you money you can't afford to lose. Review your Value-Based Purchasing (VBP) performance gaps because strong quality scores can offset rate reductions.
Days 31-60: Implementation Phase
Launch your highest return-on-investment improvements immediately. This isn't the time for analysis paralysis. Focus on:
Technology upgrades that improve operational efficiency
Staff training on accurate coding and documentation
Referral network strengthening initiatives
Process automation for administrative tasks
Evaluate every vendor and service contract. Renegotiate where possible, eliminate non-essential services, but avoid cuts that could harm quality scores or patient outcomes.
Days 61-90: Strategic Positioning
Build strategic partnerships with hospitals, physicians, and other referral sources. Strong relationships become your lifeline when patient volume drops industry-wide. Implement robust KPI tracking systems and prepare for iterative improvements.
Most importantly, abandon strategies that aren't showing results. Double down on what's working.
Revenue Optimization Without Compromising Quality
Master Your Coding and Documentation
Every OASIS assessment error is money left on the table. CMS data shows that agencies with superior documentation practices see 15-20% better reimbursement rates per episode.
Train your clinical staff on the latest PDGM requirements. Focus especially on functional improvement measures, as CMS is adding new quality measures for activities of daily living like dressing and bathing.
Optimize Episode Management
Length of stay optimization becomes critical when every dollar counts. Reduce Low Utilization Payment Adjustments (LUPA) episodes through better patient assessment and care planning. But remember, shortcuts that harm patient outcomes will hurt your VBP scores and referral relationships.
Strengthen Your Referral Network
In a contracting market, referral relationships determine survival. Implement a systematic approach to hospital and physician engagement. Share quality data, provide excellent communication, and make referring to your agency the easiest choice for discharge planners.

Value-Based Purchasing as Your Competitive Advantage
Here's where smart agencies can actually gain ground during rate cuts. Strong VBP performance doesn't just provide bonus payments; it creates a comprehensive competitive advantage affecting marketing, recruitment, referrals, and payer negotiations.
The Home Health Quality Reporting Program rewards agencies that excel in patient functional improvement. Focus on measures like:
Improvement in ambulation/locomotion
Improvement in bathing
Discharge to community
Unplanned hospitalization rates
Agencies in the top performance tiers see significantly better financial outcomes, even with base rate reductions.
Cost Management That Actually Works
Indiscriminate cost-cutting kills agencies. You can't slash your way to success. Instead, focus on surgical cost management:
Technology Investments with Measurable ROI
Invest in systems that demonstrably improve efficiency: electronic health records that reduce documentation time, scheduling software that optimizes route efficiency, and patient monitoring tools that prevent unnecessary visits.
Supply Chain Optimization
Negotiate group purchasing contracts, implement inventory management systems, and eliminate waste without compromising patient care.
Administrative Efficiency
Automate routine tasks like billing, scheduling, and compliance reporting. But maintain the human touch where it matters most: patient care and referral relationships.


Legislative Advocacy and Industry Engagement
The bipartisan Home Health Stabilization Act of 2025 proposes pausing Medicare cuts for 2026-2027. While you can't count on legislative relief, industry advocacy matters.
Submit comments during CMS's 60-day public comment period. Join your state and national associations. Share real-world impact stories with policymakers. Collective industry pressure can influence final rule modifications.
But prepare for implementation regardless. Hope for the best, plan for the worst.
Building Long-Term Resilience
The 2026 rate cuts represent more than a temporary challenge. They signal a fundamental shift toward value-based healthcare economics. Agencies that adapt now will emerge stronger and more competitive.
Strategic Partnerships and M&A Preparation
Consider strategic alliances or succession planning opportunities. Market consolidation often creates opportunities for well-positioned agencies to acquire struggling competitors or partner with larger organizations.
Quality as a Differentiator
In a contracted market, quality becomes your primary differentiator. Agencies with superior outcomes, patient satisfaction, and caregiver stability will capture market share from competitors struggling with the cuts.
Your Path Forward
The 2026 CMS rate cuts will eliminate weak agencies and strengthen smart ones. Success requires immediate action, strategic thinking, and unwavering focus on quality outcomes.
Start your 90-day action plan today. Calculate your true financial impact, identify your highest-value improvement opportunities, and implement changes systematically. Remember, this isn't about survival; it's about positioning your agency to thrive in the new healthcare economy.
The agencies that succeed will be those that view these challenges as catalysts for operational excellence and strategic differentiation. Begin now, execute consistently, and emerge stronger.
For healthcare organizations considering strategic partnerships or succession planning during this challenging period, Senate Healthcare offers specialized advisory services to help navigate these complex decisions.
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED