Home Health Value-Based Care Gets Real: How Major CMS Rule Changes Will Hit Agency Revenue (and Your Next 12 Months)
This comprehensive guide breaks down the CY 2026 Home Health Final Rule's 1.3% payment reduction and major HHVBP Model changes that are reshaping how agencies earn value-based incentives. Learn the specific measure changes, revenue implications for $3-5M EBITDA agencies, and a 12-month action plan to turn regulatory compliance into competitive advantage. The performance spread between high and low performers can reach $1.4M annually, making this transition critical for both current revenue and future exit value.
1/8/20265 min read


The CY 2026 Home Health Final Rule delivers a 1.3% Medicare payment reduction and fundamentally reshapes how agencies earn value-based incentives through revised quality measures. For home health and hospice owners, these changes demand immediate operational adjustments to protect revenue streams and position for long-term success.
Quick-Scan Summary: What You Need to Know Right Now
Payment Impact: 1.3% net reduction for 2026 (improvement from proposed 6.4% cut)
HHVBP Changes: 3 patient survey measures removed, 4 new functional/cost measures added
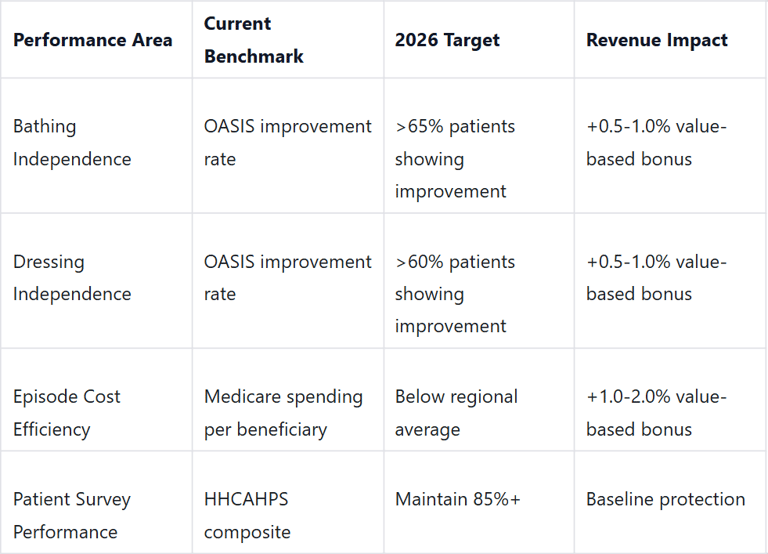
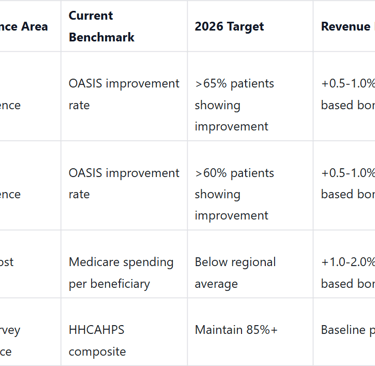
Weight Shift: Higher emphasis on bathing/dressing outcomes and Medicare spending efficiency
Timeline: New HHCAHPS survey launches April 2026 with revised questions
Revenue Strategy: Focus on functional improvements and cost containment to maximize value-based payments
Agency Impact: $3-5M EBITDA agencies face potential $40,000-$65,000 annual revenue variance based on performance
The New Reality: CMS Gets Serious About Value-Based Performance
The November 2025 Home Health Final Rule represents the most significant shift in Medicare reimbursement strategy since the Patient-Driven Groupings Model (PDGM) implementation. While agencies avoided the devastating 6.4% proposed reduction, the 1.3% cut still translates to meaningful revenue pressure for most operators.
More importantly, CMS is fundamentally changing how agencies earn value-based incentive payments. The Home Health Value-Based Purchasing (HHVBP) Model now prioritizes objective, measurable outcomes over patient satisfaction surveys. This shift reflects CMS's broader push toward accountability for clinical results and cost efficiency.


For agency owners, this creates both risk and opportunity. Agencies that adapt quickly to the new measure set can capture disproportionate value-based payments. Those that don't will face compounding revenue pressure from both base rate reductions and poor performance scores.
Breaking Down the Payment Mathematics
The 1.3% net reduction comes from several moving parts that every owner needs to understand:
Payment Components for 2026:
+2.4% standard payment update increase
-4.059% permanent PDGM behavioral adjustment (retrospective correction for higher utilization patterns)
-5.0% temporary adjustment to recoup previous overpayments
-0.5% fixed-dollar loss ratio adjustment
The temporary 5% reduction represents CMS clawing back funds from previous years where agencies received higher payments than actuarially justified. This one-time adjustment will roll off in future years, but creates immediate cash flow pressure for 2026.
For a typical $4M EBITDA agency generating $20M in annual revenue with 70% Medicare mix, this translates to approximately $182,000 in reduced Medicare payments before any value-based adjustments.
HHVBP Measure Changes: What's Out, What's In
The revised HHVBP Model removes three HHCAHPS (patient survey) measures that could no longer be calculated due to survey revisions:
Care of Patients communication measure
Communications between Providers and Patients
Specific Care Issues handling
Replacing these are four new measures focused on concrete outcomes:
Three OASIS-based functional measures targeting bathing and dressing improvements
Medicare Spending per Beneficiary for Post-Acute Care (claims-based cost efficiency measure)
This shift is intentional. CMS wants agencies focused on helping patients regain functional independence while controlling overall episode costs. The message is clear: improve real outcomes while spending less per episode.
The Weight Redistribution Game Changer
Perhaps the most significant change involves how different measure categories are weighted in the overall performance score. For larger volume agencies (typically those with $3M+ EBITDA), the weighting now favors:
Higher Weight:
Claims-based measures (cost efficiency)
OASIS-based measures (functional outcomes)
Lower Weight:
HHCAHPS-based measures (patient satisfaction surveys)
This reweighting means agencies can no longer rely primarily on patient satisfaction to drive value-based payments. Clinical outcomes and cost management become the primary drivers of financial performance.

Self-Assessment: Where Does Your Agency Stand?
Use this quick framework to evaluate your 2026 readiness:
Quick Assessment Questions:
Do you currently track bathing and dressing functional outcomes systematically?
Is your average episode cost above or below regional benchmarks?
Can your clinical team identify which interventions drive fastest functional improvement?
Do you have reliable data on post-acute spending patterns for your patients?
Immediate Revenue Implications for $3-5M EBITDA Agencies
The combination of base payment reductions and performance-based adjustments creates a significant revenue range for mid-size agencies:
Baseline Scenario (Poor Performance):
1.3% base reduction + potential 2-3% HHVBP penalty
Total impact: 3.3-4.3% revenue reduction
For $4M EBITDA agency: $660,000-$860,000 annual revenue loss
High Performance Scenario:
1.3% base reduction + potential 2-4% HHVBP bonus
Net impact: +0.7% to +2.7% revenue gain
For $4M EBITDA agency: $140,000-$540,000 annual revenue increase
The spread between high and low performers can reach $1.4M annually for agencies in the $3-5M EBITDA range. This performance gap will become increasingly important for agencies considering succession planning or sale opportunities.
Your 12-Month Action Plan
Months 1-3 (January-March 2026):
Audit current OASIS data collection processes for bathing/dressing measures
Implement systematic tracking of functional improvement rates
Analyze Medicare spending per beneficiary trends using CMS data
Train clinical staff on new functional outcome priorities
Months 4-6 (April-June 2026):
Launch revised HHCAHPS survey process (effective April 2026)
Establish monthly performance dashboards for new measures
Identify intervention protocols that drive fastest functional gains
Begin cost optimization initiatives for high-spending episodes

Months 7-12 (July 2026-January 2027):
Monitor quarterly performance scores under new weighting system
Refine clinical protocols based on outcome data
Prepare for 2027 value-based payment calculations
Document performance improvements for potential exit discussions
The Strategic Opportunity Hidden in Complexity
While these changes create operational challenges, they also present a significant strategic advantage for well-prepared agencies. The shift toward objective, measurable outcomes creates clearer differentiation between high and low performers.
For owners considering exit strategies, demonstrating consistent performance under the new HHVBP measures becomes a powerful valuation driver. Private equity buyers and strategic acquirers increasingly value agencies with proven ability to generate consistent value-based payments.
The agencies that master this transition will be positioned for premium valuations, while those that struggle will face compressed multiples and limited buyer interest. The performance spread we're seeing suggests a 15-25% valuation premium for top-quartile HHVBP performers.
Next Steps: Turn Compliance into Competitive Advantage
The 2026 rule changes aren't just regulatory compliance issues - they're revenue optimization opportunities. Agencies that view this transition strategically will emerge stronger and more valuable.
The key is moving beyond basic compliance toward building systematic capabilities in functional outcome improvement and cost management. These become sustainable competitive advantages that drive both current revenue and future exit value.
If your agency is generating $3-10M in revenue and you're looking to optimize performance under these new rules while positioning for potential strategic opportunities, this is the ideal time to develop a comprehensive roadmap.
Get started with a healthcare partnership consultation to evaluate how these changes impact your specific situation and develop an action plan for the next 12 months.
Resources:
https://oasisanswers.com/now-available-the-cms-cy-2026-home-health-final-rule/
https://healthcareprovidersolutions.com/home-health-final-rule/
https://www.cms.gov/priorities/innovation/media/document/hhvbp-exp-faqs
https://allianceforcareathome.org/the-alliance-responds-to-cy-2026-home-health-proposed-rule/
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED