7 Hospice Compliance Mistakes You're Making (and How to Fix Them Before Your Next Audit)
Hospice compliance mistakes are costing agency owners hundreds of thousands in recoupments and slashing exit multiples during buyer due diligence. This guide reveals the seven most damaging errors auditors target in 2026 and provides owner-level fixes you can implement in 90 days. If you are considering a sale or aggressive growth, your compliance posture directly impacts your valuation. Learn what clean compliance is worth and how to get there before your next audit.
1/15/20266 min read


This post covers the seven most costly compliance mistakes hospice agency owners make before audits and how to fix each one to protect your valuation, avoid recoupments, and position your agency for a successful exit or aggressive growth.
Quick-Scan Summary for Owners
Compliance failures can reduce your exit multiple by 10-20% during buyer due diligence
A single audit finding on a $3M agency can trigger $150K-$400K in recoupments
Terminal diagnosis coding errors are the #1 audit target in 2026
Documentation gaps create immediate red flags for private equity buyers
Agencies with clean compliance records command 15-25% valuation premiums
Your 90-day fix window before an audit can save six figures in penalties
Who This Is For
If you are a hospice or home health owner considering a sale, recapitalization, or aggressive growth over the next 12 to 24 months, this article is for you. Compliance is no longer just an operational checkbox. It is a direct lever on your EBITDA, your exit multiple, and whether buyers see your agency as an asset or a liability.
Buyers conducting due diligence in 2026 are scrutinizing compliance history harder than ever. One preventable audit finding can delay your deal by months or knock hundreds of thousands off your sale price. Here are the seven mistakes you need to fix now.
Mistake #1: Incorrect Terminal Diagnosis Coding
What owners get wrong: Using non-specific ICD-10-CM codes, listing symptom codes as the primary diagnosis, or utilizing prohibited Z-codes as principal diagnoses.
The financial impact: Improper terminal diagnosis coding is the top trigger for Medicare audits. A $4M hospice that faced a targeted probe review lost $280K in recoupments because 40% of claims used symptom codes instead of definitive diagnoses.
How to fix it:
Ensure the attending physician or hospice medical director certifies the terminal diagnosis
Use the most specific ICD-10-CM code available
Implement pre-submission audits to catch errors before claims go out
Train clinical and coding staff quarterly on current coding guidelines


Mistake #2: Failing to Code Related Conditions
What owners get wrong: Listing only the terminal condition on the Plan of Care while omitting co-existing conditions that impact the patient's care.
The financial impact: Missing related diagnoses leads to undercoding, which reduces your per-patient reimbursement and creates documentation inconsistencies that auditors flag. Over a 12-month period, this can represent $50K-$120K in lost revenue for a mid-sized agency.
How to fix it:
Conduct thorough reviews of each patient's complete medical history at admission
Include all clinically significant diagnoses on hospice claims
Establish clear communication workflows between clinical teams and coding staff
Use EHR systems that prompt for related conditions during documentation
Mistake #3: Misusing Combination Codes
What owners get wrong: Separately coding conditions that ICD-10-CM guidelines require to be reported with a single combination code, especially for hypertension, chronic kidney disease, and heart failure.
The financial impact: This error creates immediate audit vulnerability. Auditors view combination code misuse as a sign of inadequate compliance infrastructure, which directly impacts buyer confidence during due diligence.
How to fix it:
Invest in coding software that flags combination code opportunities
Provide ongoing staff education specific to hospice combination codes
Conduct monthly internal audits before claim submission
Document your compliance process for buyer due diligence packages
Mistake #4: Improper Code Sequencing
What owners get wrong: Listing a related condition as the primary diagnosis instead of the terminal illness, or incorrectly sequencing primary and secondary cancer codes.
The financial impact: Sequencing errors are a major red flag in MAC audits. One $5M hospice owner preparing for sale discovered that 25% of claims had sequencing issues, which delayed their transaction by four months while they remediated the problem.
How to fix it:
Always list the terminal diagnosis as the primary diagnosis on all hospice claims
Follow ICD-10-CM guidelines precisely for sequencing specific conditions
Implement quality assurance checkpoints before every claim submission
Train staff on hospice-specific sequencing scenarios quarterly
Mistake #5: Inconsistent Diagnosis Coding Across Documentation
What owners get wrong: Creating discrepancies between diagnoses listed on the Certificate of Terminal Illness (CTI), care plan, and UB-04 claim form.
The financial impact: Inconsistencies are audit magnets. When buyers review your compliance history, documentation discrepancies signal operational chaos. This alone can reduce your valuation multiple by 10-15%.
How to fix it:
Implement a standardized process to ensure consistency across all documentation
Cross-check the primary terminal diagnosis across CTI, care plan, and claim form for every patient
Utilize EHR systems that automatically populate diagnoses across documents
Establish clear communication channels between clinical staff, coders, and billing personnel
Mistake #6: Documentation and Medical Necessity Gaps
What owners get wrong: Providing incomplete documentation that fails to justify services or demonstrate why specialized hospice care was medically necessary.
The financial impact: Medical necessity gaps are the second most common reason for claim denials and recoupments. For agencies with $3M-$7M in annual revenue, this can represent $100K-$300K in annual exposure.
How to fix it:
Create comprehensive, standardized documentation policies specific to hospice care
Ensure all records clearly demonstrate medical necessity beyond simply stating a service was provided
Train clinicians to document the "why" behind every intervention
Review documentation standards as part of your exit readiness preparation
For more on positioning your agency for due diligence, see our guide on succession planning as a strategic advantage.
Mistake #7: Medication Errors and Administration Issues
What owners get wrong: Failing to properly administer prescribed doses due to miscommunication, using incorrect drug selections, improper dosages, or omitting doses.
The financial impact: Beyond patient safety concerns, medication errors create liability exposure that sophisticated buyers factor into their risk assessment. Agencies with documented medication administration issues see valuation discounts of 5-10%.
How to fix it:
Integrate electronic medication administration records (eMAR) into your digital hospice systems
Establish structured workflows with clear delegation of responsibilities
Maintain consistent team communication protocols
Conduct regular audits of medication practices and document corrective actions
Owner Mini-Examples: What Compliance Failures Cost Real Agencies
Case 1: The $4.2M Hospice That Lost $320K
A Midwest hospice owner preparing for a 2025 exit discovered during pre-sale due diligence that 35% of claims had terminal diagnosis coding errors. The buyer's legal team flagged potential recoupment exposure of $320K. The deal closed, but the owner accepted a 12% reduction in sale price to cover the buyer's risk.
Case 2: The $6M Agency That Added 18% to Their Multiple
A Southeast hospice owner invested $45K in a 90-day compliance remediation program before going to market. They implemented standardized coding workflows, EHR consistency checks, and quarterly internal audits. When buyers reviewed their compliance history, the clean record commanded an 18% valuation premium over comparable agencies with audit findings.


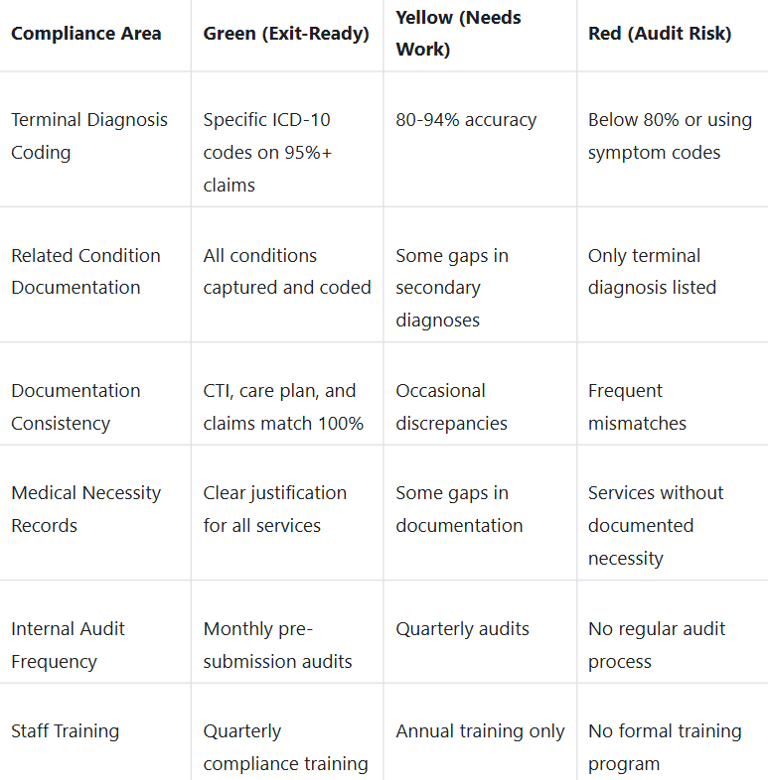
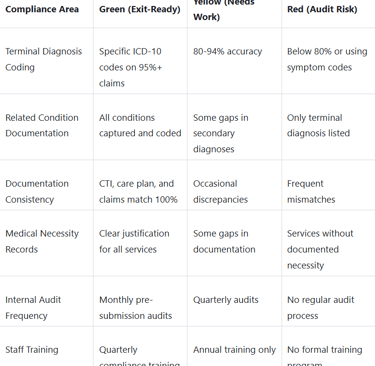
Owner Self-Assessment: Compliance Readiness Scorecard
Glossary for Owners
CTI (Certificate of Terminal Illness): The physician certification required to establish hospice eligibility
ICD-10-CM: The current diagnosis coding system required for all Medicare hospice claims
MAC (Medicare Administrative Contractor): The regional entities that process and audit Medicare claims
Recoupment: Money Medicare recovers from providers after determining claims were improperly paid
UB-04: The standard claim form used for institutional hospice billing
EBITDA: Earnings Before Interest, Taxes, Depreciation, and Amortization, the primary metric buyers use to value your agency
Valuation Impact: What Clean Compliance Is Worth
Agencies with documented compliance programs and clean audit histories command measurable valuation premiums:
15-20% premium for agencies with no audit findings in the past 24 months
18-25% premium for agencies with documented internal audit processes and staff training programs
10-15% discount for agencies with active recoupment exposure or unresolved audit findings
For more on maximizing your exit value, explore our insights on legacy planning and exit value optimization.
Your 90-Day Compliance Fix: Owner Priorities
Days 1-30: Conduct a comprehensive internal audit of coding accuracy and documentation consistency across all active patients.
Days 31-60: Implement standardized workflows for diagnosis coding, cross-document consistency, and medical necessity documentation.
Days 61-90: Train all clinical and coding staff, document your compliance infrastructure, and prepare your due diligence package.
Next Step for Owners
If your hospice agency generates $2M-$10M in annual revenue and you are considering a sale, recapitalization, or aggressive growth in the next 12-24 months, compliance readiness is non-negotiable.
Schedule a healthcare partnership consultation to evaluate your compliance posture, identify audit exposure, and position your agency to command premium valuation multiples.
Resources:
https://hospiceworks.com/hospice-compliance-mistakes-to-avoid/
https://hchb.com/10-common-hospice-medication-errors-and-how-to-address-them/
https://simitreehc.com/simitree-blog/common-palliative-care-coding-mistakes-and-how-to-avoid-them/
https://www.matrixcare.com/blog/8-most-common-billing-mistakes-in-home-health-and-hospice/
https://hospice.eewebinarnetwork.com/the-top-10-operational-structural-mistakes-hospices-make
Unlock Your 30-Minute Agency Succession Review
Maybe you're ready to expand your reach, or perhaps it's time to consider your legacy and the future of your business. Either way, it all begins with a conversation. Schedule a confidential, no-obligation call to explore what the future might hold for you and your business.
Complete the form, and we'll reach out for a chat...
© 2025 SENATE HEALTHCARE LLC.
ALL RIGHTS RESERVED